Atherosclerosis is one of the most common causes of cardiovascular diseases worldwide and the complications can be serious. The disease is characterized by the formation of atherosclerotic plaques that narrow the lumen of the arteries. Symptoms depend on which arteries are narrowed, so the manifestation of the disease can vary widely depending on the percentage of occlusion and severity.
When an artery supplying the limbs is occluded it is called peripheral arterial disease and one of the manifestations of this is called intermittent claudication. This is particularly the case when a muscle is supplied with sufficient blood at rest, but not when moving.
Clinical manifestation of intermittent claudication
Intermittent claudication (IC) is characterized by cramps and pain in the muscles with the blocked vessels that normally occur during exercise and worsen the pain until the person is forced to stop. Once the person stops blood flow, the lactic acid levels replenish, the ATP and phosphocreatine levels are reset, but ischemic damage occurs over time. The disease is classified according to the Fontaine scale, with I meaning tingling and IV critical limb ischemia.
The practical assessment for physiotherapists involves palpating peripheral pulses in the lower limbs and calculating the maximum claudication distance, this is the maximum distance a person can walk before having to stop because of their symptoms. Perhaps the simpler alternative is to ask the patient how much pain they can walk. Currently a limit of 100 m means that surgery must be considered.
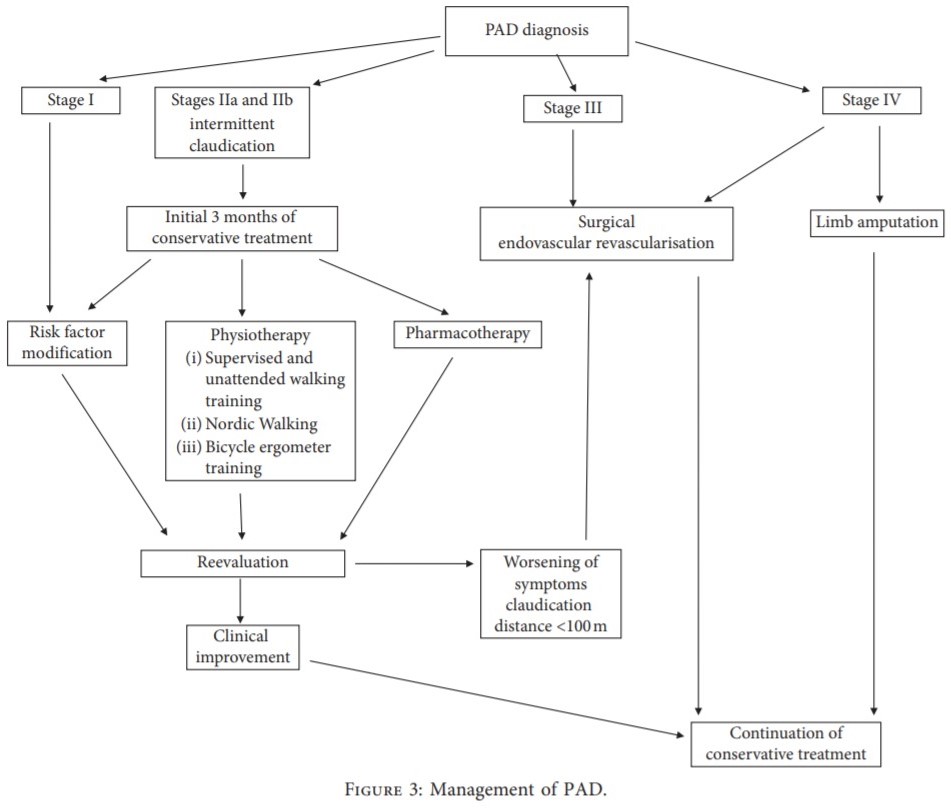
Physiointervention for IC – A flow chart
If IC is suspected, you should contact a vascular surgery department for an appropriate diagnosis and first aid. If you have been referred to you through a vascular surgery / study, you must ensure the following:
the location of the stenosis was recognized,
the stage of ischemia has been clarified,
the initial and absolute claudication interval as well as the type of treatment (pharmacological or surgical) are determined; and
coexistence diseases and
Contraindications for certain rehabilitation methods are known.
Only then can an individual, personalized outpatient rehabilitation program be designed for each patient.
The overall topic of treatment is to improve the quality of life by relieving pain in the limbs when walking and reducing the risk of cardiovascular complications. Therefore, monitored walking training on a treadmill is the best initial treatment for patients with IC.
Training units should last 30 to 60 minutes and take place 3 times a week for at least 3 months. The suggested belt speed is 3.2 km / h with increasing incline of a treadmill. At the same time, it is emphasized that the maximum pain of the ischemic muscles when walking should always be avoided. If the symptoms improve, the duration and speed of the sessions can be slowly increased.
Outside of physio sessions
Outside of the sessions, patients should be encouraged to walk “a lot, but not with force” as walking should be painless. It should be emphasized that if the patient feels severe pain and muscle cramps while walking, this has very negative consequences as a result of ischemia – reperfusion injury (IRI).
If patients find it difficult to walk due to competing comorbidities, cycling on a static bicycle with the forefoot on the pedals instead of the metatarsus should be encouraged. This is to ensure greater crural movement during exercise. This, too, should be pain-free, as when walking, and rest is obligatory when pain sets in and the exercise can be continued after calming down.
It goes without saying that in addition to smoking cessation and a change in diet, education about arteriosclerosis is essential. Lifestyle advice should never be underestimated for people with peripheral vascular disease and even for patients before they reach the stage of IC symptoms.
This entry was originally published in November 2019 and written by Scott Buxton . The page has now been updated to ensure that it is up-to-date, accurate and complete.