Sarcopenia should be viewed as a disease; acute or chronic muscle failure. Identification and management should be a priority and central goal of every physical therapist in treating the elderly.
With increasing age, our muscles change progressively, which mainly leads to a loss of muscle mass and strength. The age-related loss of muscle function is known as sarcopenia and is derived from the Greek words for meat (sarcos) and loss (penia). Its definition includes loss of muscle strength and strength, and decreased function. It occurs with age and is a major component in the development of frailty.
The SARC-F questionnaire is recommended by EWGSOP 2 for characterizing sarcopenia. This is a self-reported 5-point questionnaire with low to moderate sensitivity and very high specificity. It's inexpensive, convenient, and ensures doctors identify severe cases of sarcopenia. Hence, it is a great tool for introducing the concept of muscle failure into clinical practice.
There are a number of studies with which the severity of muscle loss in older adults can be reliably quantified, but these are expensive and unavailable for 99% of practicing physicians. They are interesting nonetheless and are likely to become more commonplace in the future.
Take CT scans of the 3rd lumbar spine as an example. L3-CT correlates significantly with the muscle mass of the whole body and accurately predicts the prognosis. CT is also useful for examining muscle mass in the middle of the thigh, which may be more accurate than L3 CT.
A cheaper and just as accurate alternative to CT is diagnostic ultrasound (USS) and it is extremely reliable. USS will also inform the user about muscle thinness, cross-sectional area, fascicle length, pennation angle and echogenicity, which is sure to make all physios jump for joy. The European Geriatric Medical Society is preparing a consensus protocol for the US application in sarcopenia so that it can be used in the near future, at least in research to diagnose sarcopenia.
Sarcopenia: EWGSOP2 algorithm for case identification, diagnosis and quantification of the severity in practice. The steps of the path are shown as Find-Assess-Confirm-Severity or F-A-C-S. * Consider other reasons for poor muscle strength (e.g. depression, stroke, balance disorders, peripheral vascular disorders).
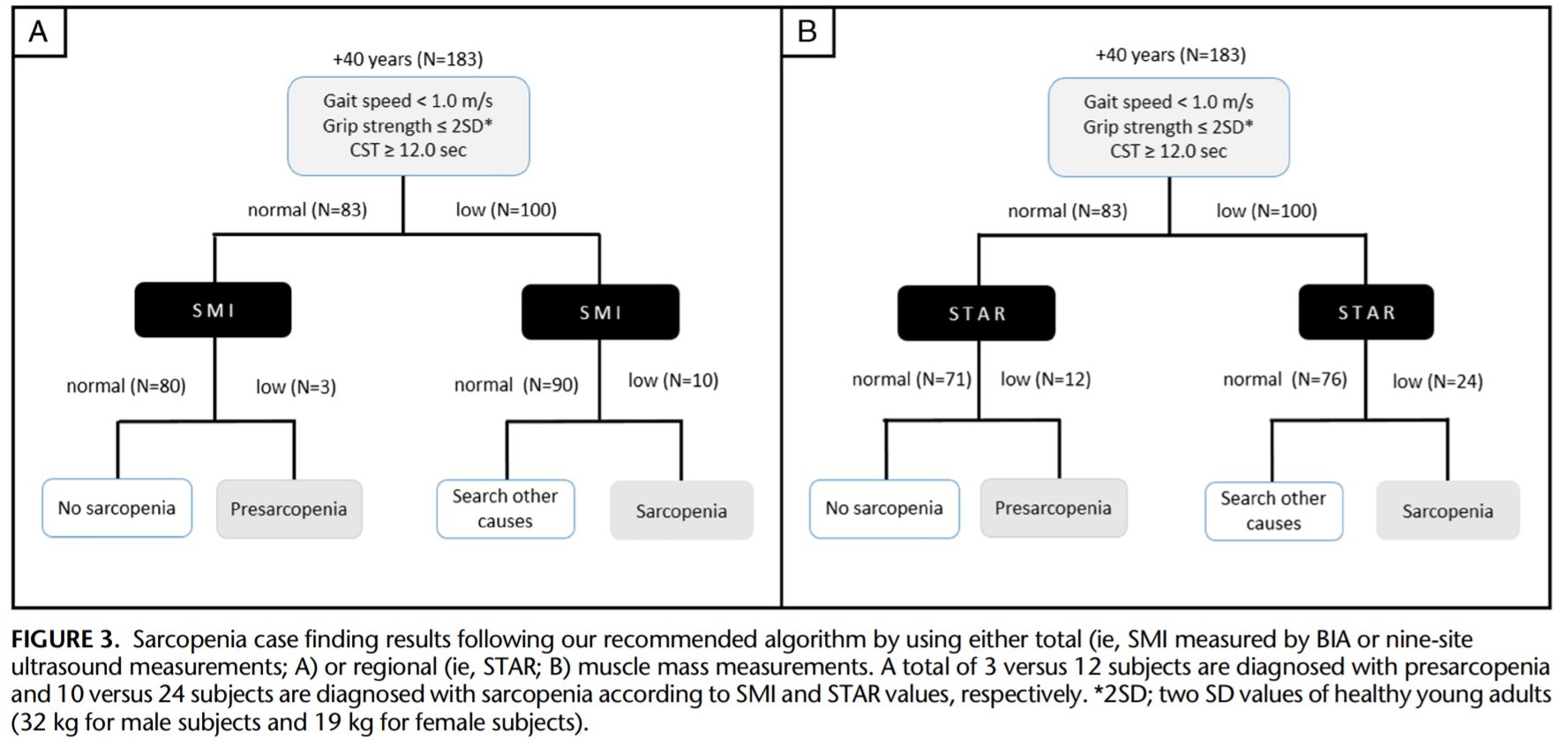
A new cross-sectional study with 326 adults was published in which the applicability of USS in diagnosis in a clinical setting was examined. In particular, the regional muscle mass measurement of the quadriceps using the STAR measurement instead of the whole body measurement can be used reliably in the diagnosis of sarcopenia. Interestingly, this could aid early detection as well, but more studies are needed to confirm this hypothesis.
STAR = anterior thigmuscle thickness (mm) / BMI (kg / m2)
Clinical implication
The anterior thigh is often the first muscle mass to be affected by the sarcopenic process and therefore the most likely candidate for a consistent and possible early diagnosis. This study examined the scores using the USS and STAR measurements, and a score of 1.0 (female) and 1.4 (male) appears to be useful for diagnosis.
Introduction to Frailty
 Frailty is a clinical condition that is associated with many negative outcomes, including falls, accidents, and disability or death. It is estimated that 25-50% of the population aged 85 and over can be classified as frail and therefore most physical therapists encounter frail patients. In this course, you will learn about frailty and gain important insights into the effects it has on patients and their quality of life.
Frailty is a clinical condition that is associated with many negative outcomes, including falls, accidents, and disability or death. It is estimated that 25-50% of the population aged 85 and over can be classified as frail and therefore most physical therapists encounter frail patients. In this course, you will learn about frailty and gain important insights into the effects it has on patients and their quality of life.
How is sarcopenia related to frailty?