The exact identification of the far-reaching systemic effects of spondyloarthropathy is the key to enabling early detection.
With many rheumatological diseases there are considerable delays in diagnosis. These delays consequently affect accurate, timely treatment and subsequent intervention, and most importantly affect the quality of life of people living in these stressful conditions. The UK Society for Rheumatology (BSR, 2015) has published a strategy report outlining the main challenges and opportunities for rheumatology services in the UK. They emphasized the importance of an early diagnosis and suggested a “12-week time window” in which patient care can be positively influenced by appropriately addressing a rheumatologist within this period.
In addition, a national rheumatoid arthritis and early inflammatory arthritis clinical audit was conducted with the aim of evaluating the early treatment of patients referred to rheumatology providers with suspected inflammatory arthritis in England and Wales. The audit confirmed that most people with early inflammatory arthritis wait too long from the onset of symptoms to the onset of disease-modifying treatment. The review also found that there were frequent delays in referring GPs and then further delays after their first referral. I would go further to conclude that delays also occur in the physical therapy practice.
In general, intra-articular features that are suspicious of synovitis and systemic inflammation are clear and are often noted; For example, the most important signs of inflammation (erythema, heat, edema) as well as pain, stiffness and restricted mobility. However, extra-articular manifestations (EAMs), those that are or occur outside of a joint, are often less well known.
Extra-articular manifestations are the key to early detection
In addition, these EAMs prove to be particularly elusive if:
Symptoms are palindromic (flare and do not return for some time)
The symptoms imitate the state of the musculoskeletal system or merge unnoticed between several rheumatic diseases
Patients cannot identify symptoms as related to rheumatology
There is a low index of suspicion for systemic inflammatory conditions
It is then easy to see why there are longer delays in diagnosis for some of these conditions. The delay is still around eight years for some conditions, such as axial spondyloarthritis (axSpa, formerly known as ankylosing spondylitis, AS), and there is a lot we could do to change that.
Physiotherapists have the option of believing having a possibility to recognize the signs and to quickly point out the appropriate path for the benefit of the patient with current instructions.
But where should I start? I propose the following:
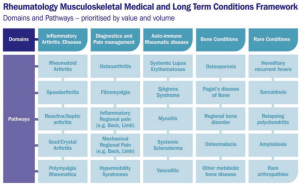
Development of awareness of rheumatological diseases
Develop your inflammation pattern recognition
Note Extra-articular manifestations
Awareness of rheumatological conditions
Summary and take away key
Patients with inflammatory diseases of the musculoskeletal system often face physiotherapists in a number of situations that disguise themselves as a “mechanical” condition . For me, the exciting aspect of our role is deciphering these disguised symptoms, considering whether there really is a rheumatological element. By looking more closely at rheumatological conditions and their intra- and extra-articular manifestations, we as clinicians are in agreement with current knowledge and best practices.
Intra- and extra-articular manifestations are indications of a systemic inflammatory etiology, but we must of course be careful. We risk flooding our medical colleagues with inquiries to take our suspicions into account ; Insertion Achilles tendinopathy can easily be confused with rheumatological enthesopathy.
Nevertheless, in my opinion we still have to be suspicious. If we lead the thoughts and discussions successfully, we, as physical therapists, can help change the direction of care for people with rheumatological diseases and will further advance timely, accurate diagnosis, treatment and treatment.
This entry was originally published in June 2017 and written by Chris Martey . The page has now been updated for freshness, accuracy and completeness.
References
British Society for Rheumatology (2015) The State of Rheumatology in Britain: Insights into the Pressures and Solutions of the Service. [Accessed 11th May 2017 https://www.rheumatology.org.uk/Portals/0/Policy/Policy%20Report/Rheumatology%20in%20the%20UK%20the%20state%20of%20play.pdf].
British Society for Rheumatology (2016) National Clinical Audit for Rheumatoid and Early Inflammatory Arthritis: A Guide for Patients and the Public. [Accessed 11th May 2017 https://www.rheumatology.org.uk/Portals/0/Policy/Audit%20reports/Patient%20guide%20-%20national%20clinical%20audit%20for%20rheumatoid%20and%20early%20inflammatory%20arthritis%20-%20second%20report.pdf]
Brukner, P. & Khan, K. (2012) Clinical Sports Medicine. 4th edition, McGraw-Hill Australia Pty Ltd. Australia.
Kalappan, M., Abubacker, N. R. T., Shetty, M., Rajendran, K., Rathinam, W. K. M. and Karuthodiyil, R., 2017. Investigation of extra-articular manifestations and disease severity in patients with rheumatoid arthritis. International Journal of Advances in Medicine, 3 (1), pp. 53-56.
Ledingham, JM, Snowden, N., Rivett, A., Galloway, J., Ide, Z., Firth, J., MacPhie, E., Kandala, N., Dennison, EM and Rowe, I. , 2017. Achieving NICE Quality Standards for Patients with Emerging Inflammatory Arthritis: Observations from the National Clinical Audit for Rheumatoid and Early Inflammatory Arthritis. Rheumatology, 56 (2), pp. 223-230.
Pieren, A., Peiteado, D., de Miguel, E., Espinel, M., Moral, E., Monjo, I., Paredes, MB, Tornero, C., Bonilla, G., Plasencia, C. and Nuño, L., 2016. FRI0405 Extra-articular manifestations in patients with spondyloarthritis receiving biological treatment. Annals of the Rheumatic Diseases, 75 (Suppl 2), pp. 582-582.
Siegel, E.L., Orbai, A.M. and Ritchlin, C. T., 2015. Targeting extra-articular manifestations in PsA: a closer look at enthesitis and dactylitis. Current opinion in rheumatology, 27 (2), pp. 111-117.
Singal, A. and Arora, R., 2015. Nagel as a window for systemic diseases. Indian Dermatology Online Journal, 6 (2), p.67.
Stolwijk C, van Tubergen A, Castillo-Ortiz JD. (2015) Prevalence of Extra-Articular Manifestations in Patients with Ankylosing Spondylitis: A Systematic Review and Meta-Analysis Annals of the Rheumatic Diseases; 74: 65-73.
Websites [accessed May 2017]: www.arthritisresearchuk; www.nass.co.uk; www.rheumatology.org.uk