The international framework for the examination of the neck region for possible vascular pathologies of the neck before manual therapy has been updated. We have summarized the most important clinical take-homes for you.
The framework is intended to provide guidelines for the assessment of the C-spine for possible vascular pathologies of the neck prior to the planned mobilization, manipulation and movement. The first edition was released in 2012 and although a revision is planned for 2017, an update has now been released.
The reason we need this document is that since the beginning of manual therapy in the past, there have been neurovascular safety incidents in patients in connection with the use of the therapy and, more recently, the appearance of vascular masquerades. These are arterial pathologies that can potentially appear as MSK pain and dysfunction. Therefore, the aim of this document is to improve the clinician's understanding of risk and pathology to ensure safety.
Messages to take away
Incidents are rare, but not impossible or outrageous. Therefore, adherence to this framework is strongly recommended
The cervical artery dysfunction (CAD) has been replaced by vascular pathologies of the neck
Provocative position testing is not recommended; instead, clinicians should build a suspicion index based on a solid subjective assessment
There is not a single test to test a vascular hypothesis. Therefore, it is important to understand the patient's presentation
The aim of the document is not to provide you with a protocol of compliance, but rather to improve the clinician's understanding of risk and pathology to ensure safe practice
The rate of vertebral artery dissection (VA) in the general population is estimated to be 0.75 to 2.9 per 100,000.
Internal carotid artery (ICA) dissections are 3-5 times more common.
The majority of serious adverse events related to manual therapy and the neck involve the VA rather than the ICA.
Deep immersion in vascular risk factors with Roger Kerry
Method behind the update
The framework is a consensus document that was created through a series of robust evidence-based phases.
A survey evaluating the 2012 Framewrok was distributed to all IFOMPT affiliates and stakeholders in 2016.
The key issues identified in the survey were first examined at the IFOMPT conference in 2016. The survey was used to facilitate discussion and the result was the need to update the framework. Initial revisions were made after discussions, then SRs and guidelines were used to inform the updated framework, and if no evidence was available consensus was used.
The iterative consultation on the draft was used and passed on to professional member organizations, IFOMPT interest groups, international experts, as well as osteopaths and chiropractors. The final design was reviewed by a doctor specializing in stroke and interventional neurology.
Vascular pathologies
There are a number of vascular diseases that all therapists should know, many of which are musculoskeletal pain. So it is important that this is taken into account in your assessment. The following table is taken directly from the framework document and all information on the pathologies can be found in Physiopedia.
Subjective history and risk factors
Rarely is an event associated with a single causal factor, instead they are usually complex and mutifactorial, which makes it difficult to know for sure. However, risk factors are known that increase the likelihood of vascular pathology in patients and are therefore contraindicated for manual therapy without further investigation. These must be known to the clinician and directly determine the likelihood of suspicion.
There are no definitive tests as the presentations can be very different. However, there are some similarities that clinicians should be aware of. Both risk factors and signs and symptoms are detailed in the infographic below.
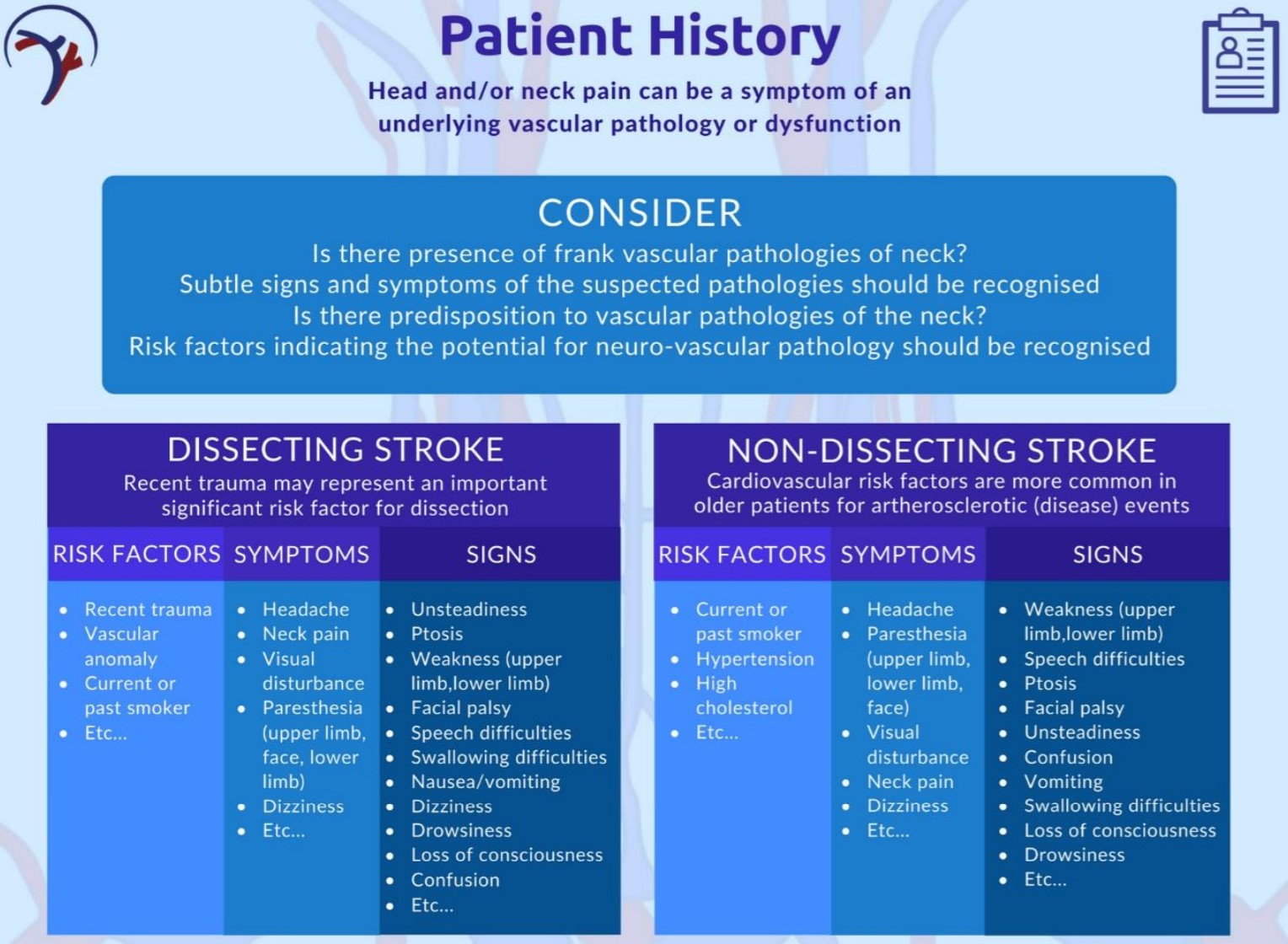
It is important to remember that spontaneous dissection events are not associated with historical risk factors. Therefore, clinical reasoning must recognize that the absence of risk factors does not absolutely rule out a serious neurovascular event.
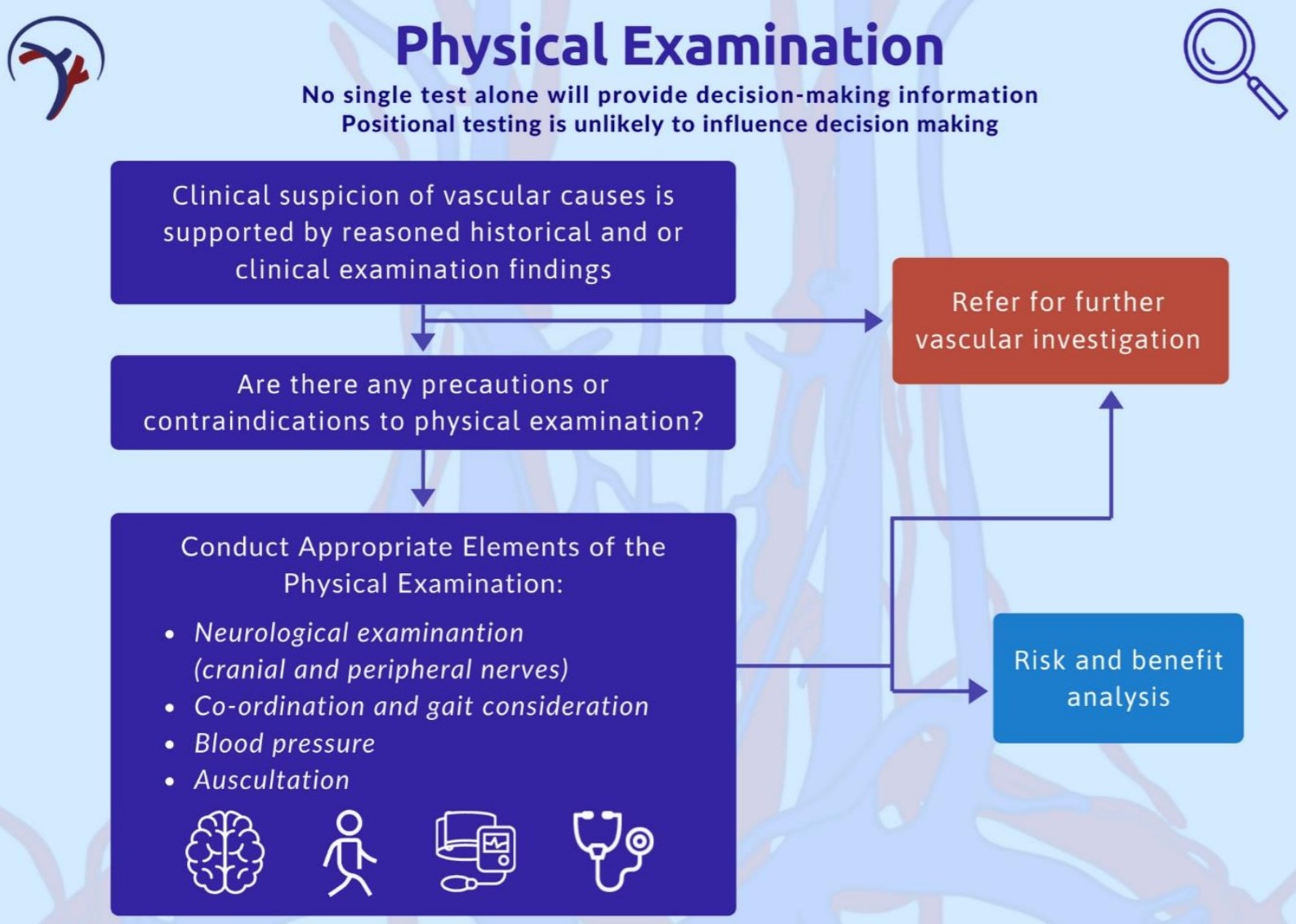
Physical examination
Always remember the aim of your objective assessment, which is to test the hypothesis generated in the subjective story. The outcome of the history and examination in the case of this framework is to determine whether or not another referral to a doctor is warranted. A specific diagnosis is not required, but a decision whether or not to reprocess the vascular system, or whether to reprocess it with physiotherapeutic intervention.
An essential part of the physical examination consists of creating a suspicion index and testing the vascular hypothesis. Three specific examination techniques are recommended by the framework
:
Blood pressure
The aim of measuring blood pressure is to determine the risk of stroke and acute arterial trauma. Hypertension is a strong predictor of CVD but needs to be interpreted in conjunction with other findings. It is also important to remember that there is not a discrete threshold, but a correlation; H. The higher the blood pressure, the higher the risk of vascular pathology.
Neurological examination including cranial nerves
The aim of a neuro-examination in this context is to add supporting evidence to your vascular hypothesis. An example of this could be paresthesia or a change in facial sensation, which could be a sign of a non-dissecting stroke. Another example could be vision loss with scalp tenderness in giant cell arthritis.
Examination of the carotid artery
This includes both palpatation and auscultation of the carotid. A change in heart rate has been identified as a feature of internal carotid disease, and asymmetry between left and right vessels is considered significant. A pulsating, expandable mass indicates an arterial aneurysm. At auscultation, a fruit indicates a significant finding and should be correlated with the rest of the test results.
With all the clinical recommendations in the frame, there are some infographics that allow easy digestion and reference within clinical practice. The physical exam is below.
Risk & benefit
As with all treatment options, the risk and benefit must be assessed. This is especially important for manual neck therapy for all of the reasons mentioned in this article. It is difficult to express the relationship between risk and benefit as it would require a huge prospective database with hundreds of thousands of patient records. It's just not doable. Therefore, the assessment of risk and benefit relates to the risk-related relationship with the treatment, not to a misdiagnosis.
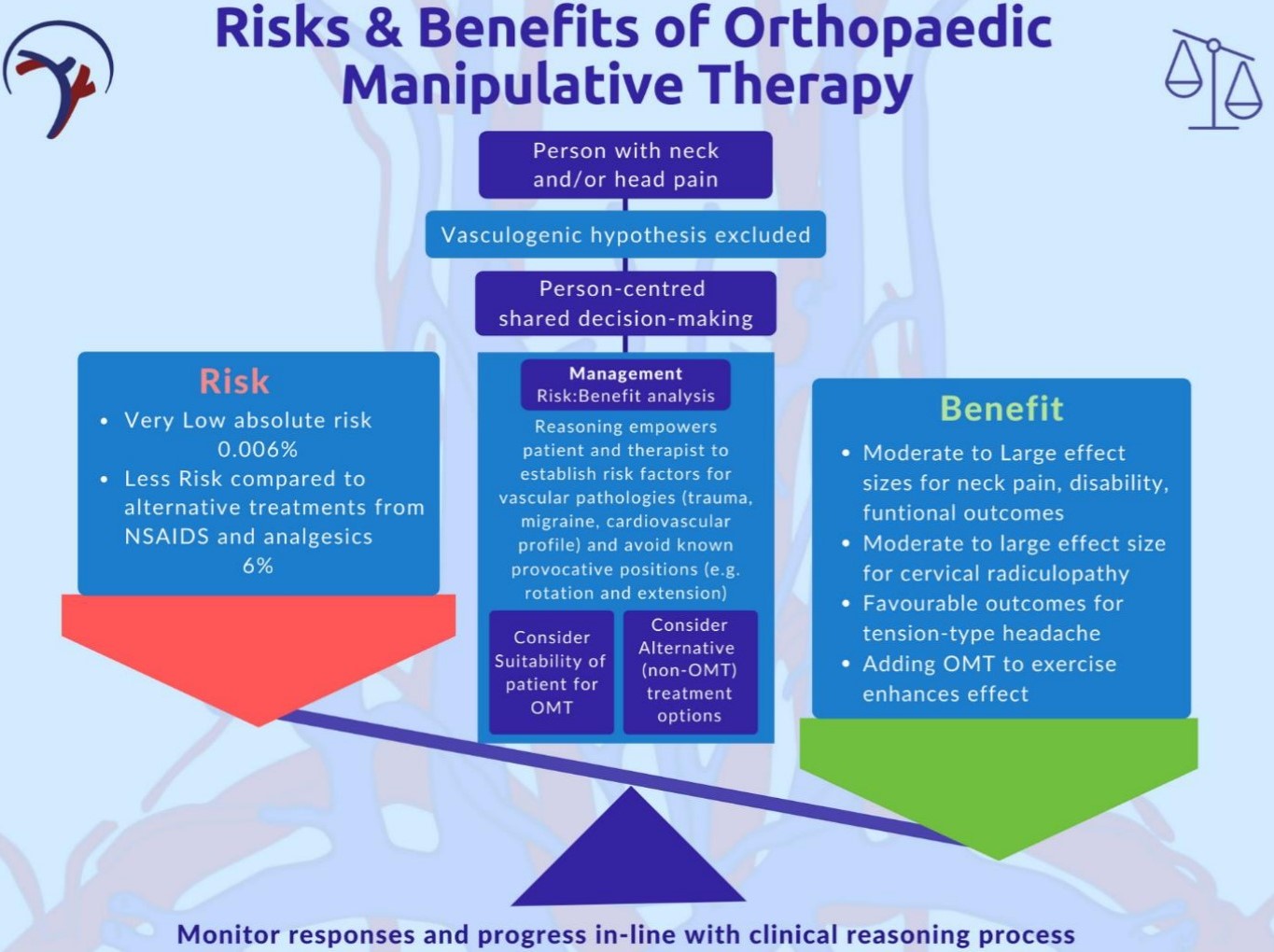
It is the responsibility of the physiotherapist to recognize and check whether a patient poses an increased risk and to minimize this. The two main risks are:
The risk of misdiagnosis of an existing vascular pathology
The risk of serious adverse events after manual therapy
The main hypothesis is that the patients who have head / neck pain and continue to experience a serious adverse event, i. H. Having a dissection, an underlying pathology made worse by treatment. It is therefore the responsibility of the physical therapist to reduce this risk by taking into account as far as possible known risk factors, signs and symptoms that are described in this context.
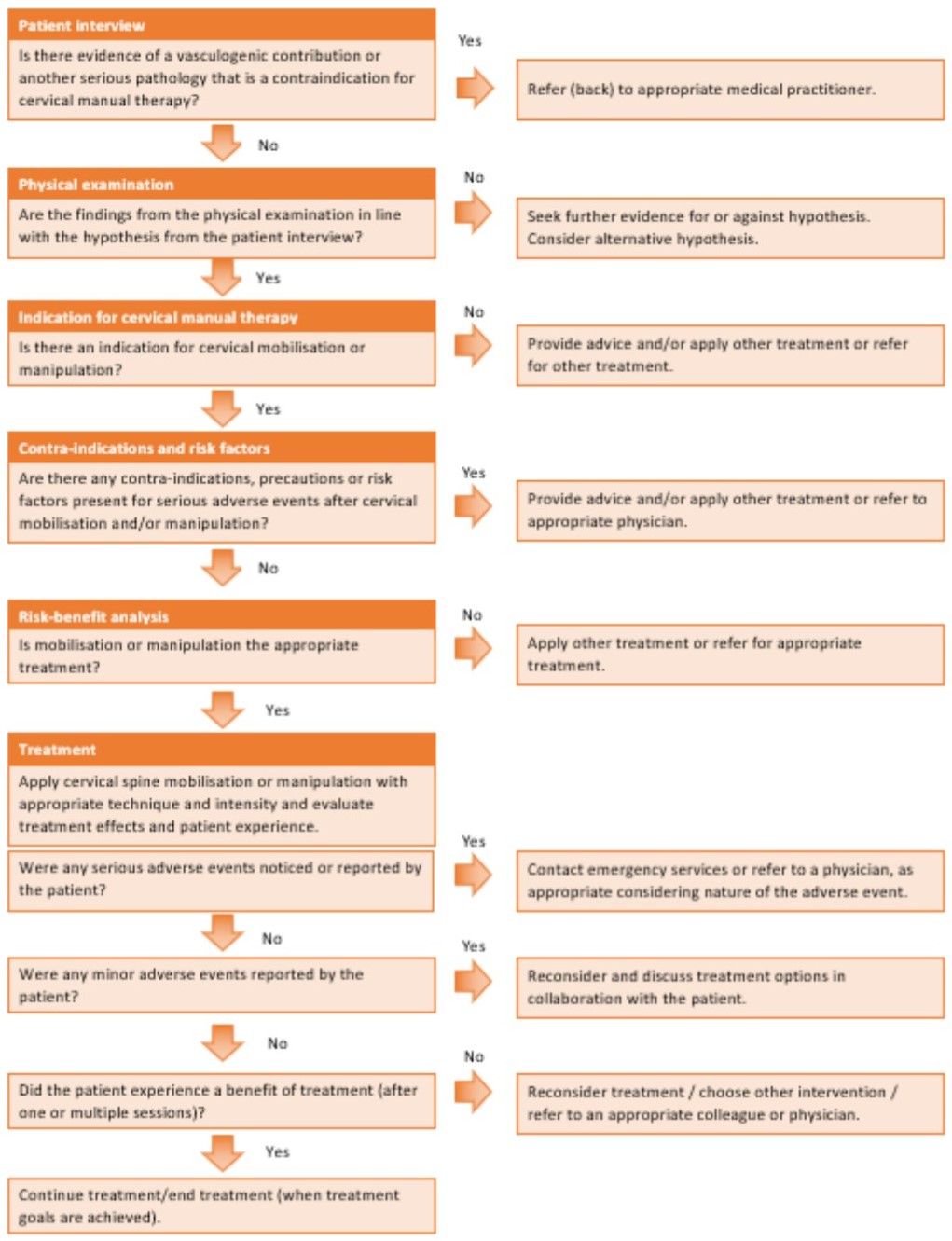
Flowchart for clinical thinking
Other parts of the frame
The rest of the framework contains details on the following areas:
Lesson recommendations for trainers
Medical framework and shared decision making
What a safe manual therapy practice looks like
Deep dive into vascular pathology with Roger Kerry
 Neck vascular pathologies are used in physiotherapy to cover a variety of vascular pathologies that can restrict blood flow to the brain. When evaluating and treating the cervical spine, it is important to understand blood vessel disorders that can be associated with pain and to assess the risk of a patient experiencing restriction in arterial flow during a physiotherapy evaluation or treatment. In this course, Roger Kerry teaches you how to make safe clinical decisions that take these very serious issues into account and how to update the appropriate framework for clinical practice.
Neck vascular pathologies are used in physiotherapy to cover a variety of vascular pathologies that can restrict blood flow to the brain. When evaluating and treating the cervical spine, it is important to understand blood vessel disorders that can be associated with pain and to assess the risk of a patient experiencing restriction in arterial flow during a physiotherapy evaluation or treatment. In this course, Roger Kerry teaches you how to make safe clinical decisions that take these very serious issues into account and how to update the appropriate framework for clinical practice.
Make Safe Clinical Decisions Roger Kerry