We know that back pain is the most common cause of disability worldwide. Over half a billion people live with back pain every day. About 75% of people will have at least one episode of back pain in their lifetime, and a large proportion (~ 25%) will develop chronic pain .
Many primary care patients in primary care for their back pain and a stratified approach to management of care have been shown to be effective in reducing the number of patients who experience chronic problems.
Research stratified care for LBP
The evidence for a stratified approach has been well studied in European health systems and has been shown to be effective. However, a US study published in 2018 was unsuccessful when using the layered approach. A new study published this week re-examined this in a US population.
The aim of the TARGET study was to test whether the implementation of a risk-stratified approach to the treatment of back pain in primary care would lead to lower results for chronic lower back pain and improved self-reported disability in the USA.
]
Methods
The TARGET study was a randomized controlled multi-site cluster study with a 1: 1 allocation ratio. The cluster locations were 5 primary care clinics in the US; UPMC, BMC, JHM, IH and MUSC. These clinics were randomized into two groups – one was general care and the other was general care + psychologically informed physical therapy.
Patients aged 18 and over who presented themselves to participating hospitals for basic care with a primary complaint of acute pain in the lower back were able to take part in the study. If the pain was present for more than 3 months, or if the pain had prevented daily activities more than every other day, participants were excluded as this classified them as chronically symptomatic.
All remaining participants then completed the STarTBack tool which divided participants into a high risk group (score 4 or more), a medium group or a low risk group. These high-risk patients were included in the study and randomized to either standard care or standard care + psychologically informed physical therapy.
The study was of a pragmatic nature, which meant that the standardization of psychologically informed physiotherapy was not closely monitored, but a treatment checklist was developed and used by the clinicians involved in the study. This clearly has an impact on the results, but is more representative of the variable practice in real clinical situations on a daily basis.
The primary result for the study was the patient-reported transition from acute to chronic pain in the lower back and a disability associated with back pain after six months (ODI). Secondary results were medical utilization over 12 months from the first assessment as measured by outpatient visits, imaging inquiries, pain procedures, and hospital admissions.
The log for the process can be read in full on pubmed.
Results & clinical significance
A total of 77 clinics at 4 locations were randomized and 2,300 participants were recruited, 1207 of them in the intervention group and 1093 in the control group. Interestingly, during the screening phase for suitability 50% of the patients already had chronic back pain that is above the current estimates in the USA . During this screening phase, 36% had a low risk, 40% a medium risk, and 55% a high risk of developing persistent (and therefore chronic) back pain.
Much has been said about the opioid epidemic in the United States, and on the first visit, 22-25% of the high-risk group were given opioids, 40% for muscle relaxants (non-specific), and 30% for NSAIDs – all of which we know they are largely ineffective for back pain when used for longer than the early stages of an acute episode. After 1 year, 8% continued to take opiates.
Basic concepts of analgesia
If you consider that only 57% of the participants in the intervention groups had a referral for physio or physio + psychological intervention, but 25% received opiates are an indication of an excessive dependence on painkillers – it is too easy to accept the prescription Before looking for alternative remedies, get pain management first. This contradicts all recent clinical guidelines for back pain.
Brief summary of the TARGET process
Stratified Care has been shown to be effective in European health systems but this is the largest study examining its effectiveness in the USA.
8% of the participants in the high-risk group were still taking opiates after 1 year.
Only 5% of the patients were referred to non-medical specialists during the initial examination .
51% of the participants in the intervention group switched to chronic pain
48% of the participants in the control group switched to chronic pain.
Only 5% of the participants in the initial consultation received a referral to a non-medical specialist for back pain . This is interesting, and unfortunately the subgroup analysis of these patients is not detailed enough to be analyzed further.
]
At the 6-month point in time, around half of the patients in both groups stated that they switched to chronic pain, with 70% impairing their daily life. This is shown in the following bar graph.
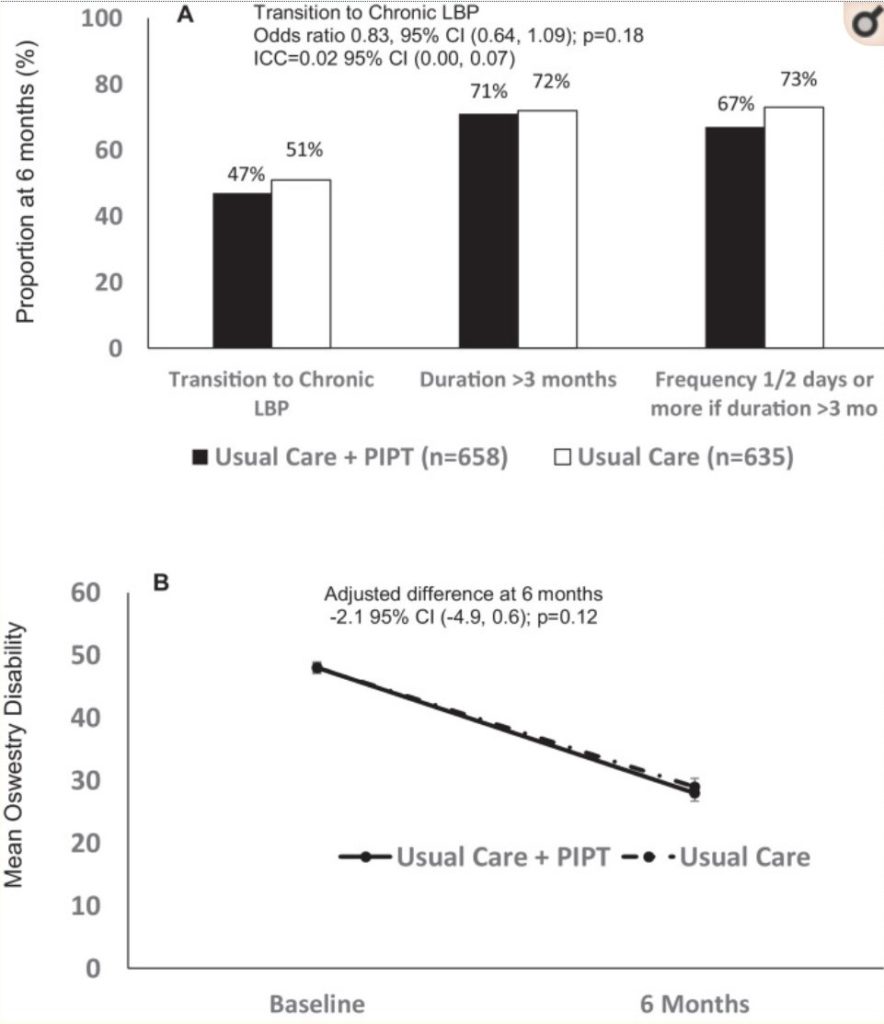
According to the ODI, however, there was an overall reduction in the number of participants with severe disabilities, which indicates a certain degree of success in the interventions, especially in the psychologically informed treatment group. However, this success did not reach any clinical or statistical significance for any of the groups after 6 or 12 months. It is entirely possible that the participants who went on to chronic pain adjusted their lifestyle to live with the pain as much as possible, thereby lowering their ODI values.
In summary, 51% of the participants in the intervention arm and 48% of the participants in the control arm switched to chronic back pain, which indicates no significant difference in the results between the two groups. The change in the ODI value is likely due to people adapting their lives to life with chronic pain. However, this is unclear given the details given in the study.
Stratified treatment for back pain has been shown to be effective in European health systems, but this clearly cannot be said for the United States of America. Other cultural and economic factors likely play a role here, such as insurance, access to specialists and the current over-dependence on opiates.